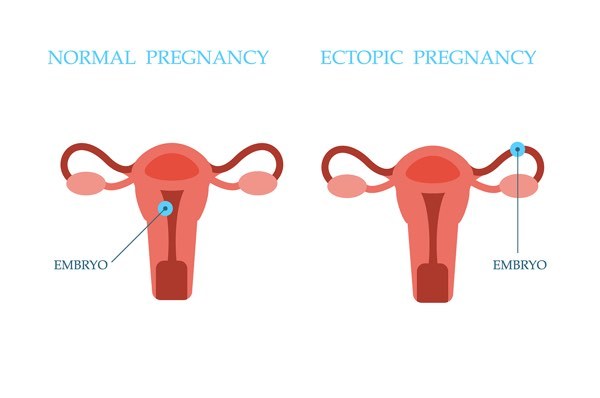
Pregnancy can be a smooth journey or you can be confronted with complications like concerns over ectopic pregnancy (pregnancy outside the uterus) and miscarriage. Concerns in early pregnancy are valid as 1 in 4 confirmed pregnancies end in miscarriage before 20 weeks but only 1%-2% of miscarriages are a result of ectopic pregnancy.
Signs of an ectopic pregnancy
Often I am contacted by expectant mothers worrying about troubling signs of miscarriage in the first trimester – especially if this is their first pregnancy or they have had trouble falling pregnant.
A big concern a lot of pregnant women have is vaginal bleeding in early pregnancy. Occasional spotting or light bleeding in the very early stages of pregnancy is something a lot of women experience. Vaginal bleeding can also be a symptom of an ectopic pregnancy.

Here are other symptoms of an ectopic pregnancy:
- Persistent and severe abdominal pain, usually on one side
- Vaginal bleeding or spotting, commonly after the pain has started
- Pain in your shoulder tip
- Diarrhoea and vomiting
- Feeling very faint and light-headed, and possibly fainting
Pregnant women with an ectopic pregnancy may have one or several of these symptoms. If you are experiencing any of these symptoms it is important to visit your doctor immediately.
Diagnosis of an ectopic pregnancy
An ectopic pregnancy is established by a pelvic exam, ultrasound and blood tests. Typically, a pelvic exam detects tenderness in the uterus or fallopian tubes but little else. A transvaginal or abdominal pelvic ultrasound will show where the pregnancy is located if the pregnancy is far enough along.
For most, blood tests for the pregnancy hormone (human chorionic gonadotropin or hCG) levels are taken 48 hours apart for low or slowly increasing levels of hCG in the blood which would suggest early abnormal pregnancy, such as an ectopic pregnancy. Let’s start with the fact that early diagnosis and treatment of ectopic pregnancy is critical to saving your life. Ectopic pregnancy causes 10% of deaths in the first trimester.
What happens after an ectopic pregnancy diagnosis?
When it comes to an ectopic pregnancy, the major concern is for the mother’s safety. If an ectopic pregnancy is detected immediate action needs to be taken to avoid rupture and life-threatening blood loss.

Treatment Options
A very early and declining ectopic can be managed with a ‘wait and see’ approach. In some cases, treatment is taking a medicine called methotrexate to end the pregnancy and avoid surgery and general anaesthesia. If methotrexate is not an option then minimally invasive laparoscopic surgery is commonly used to treat ectopic pregnancy, especially if tubal rupture is suspected and the mother’s life is in danger.
Post Treatment Management
After treatment your doctor will regularly test your blood to make sure that your pregnancy hormone (hCG, or human chorionic gonadotropin) levels are dropping.
I would advise that couples wait until after physical and emotional healing before trying to get pregnant again. Women who have had an ectopic pregnancy are at slightly higher risk of another ectopic pregnancy (1 in 10).
Now, if you are in your first trimester (first 12 weeks) and you are having any of the signs of ectopic pregnancy ask your GP for a referral to me or a gynaecology specialist immediately.
Useful links
Experiencing Fertility problems? Or maybe you have had a miscarriage and don’t know where to go from here?